The discussion within the scientific and medical community around the topic of intestinal bacteria, or the intestinal microbiome, is currently very alive. A good example of this heated arena is the work of Rob Knight, lead investigator of the Human Microbiome Project. A lot of important data and potential therapeutic models are being developed out of this project. Before I get into the fascinating and inspiring implications of recent microbiome studies, let’s take a step back and look at what intestinal bacteria is, how it affects your health, and whether certain types are beneficial.
What Is Intestinal Bacteria?
Intestinal bacteria, also known as gut flora, consists of a complex community of bacteria and microorganisms that live in the digestive tracts of humans and animals. This community makes up the intestinal microbiome—a very important subset of the human microbiome. It plays a large role in digestion and your body’s ability to break down various types of food. Check out the Foundation for Human Nutrition: Part IV to learn more.
What Impact Does It Have on Human Health?
The variety, volume, and relative balance of the intestinal bacteria population within the gut definitely has a huge correlation with human health. Over the past few years, intestinal microbes have been linked to a wide range of diseases. Asthma, eczema, allergies, irritable bowel syndrome, colitis, heart disease, diabetes, obesity, depression, anxiety, and autism all share the common feature of a bacterial imbalance in the intestine.1-7 The intestinal microbial community indeed seems to have a great impact in terms of its connection to individual diseases, as well as its relationship to overall health. The body of research currently in development has many positive implications. One of the most inspiring examples is the successful treatment of C. diff (bacterial chronic diarrhea) using fecal implants. By taking samples of intestinal bacteria from healthy individuals and transferring them to individuals with C. diff, scientists have been able to totally cure this disease—with 98% reliability.
For more information, watch Rob Knight’s TED Talk on “How Our Microbes Make Us Who We Are.”
So Are Certain Types of Bacteria Good?
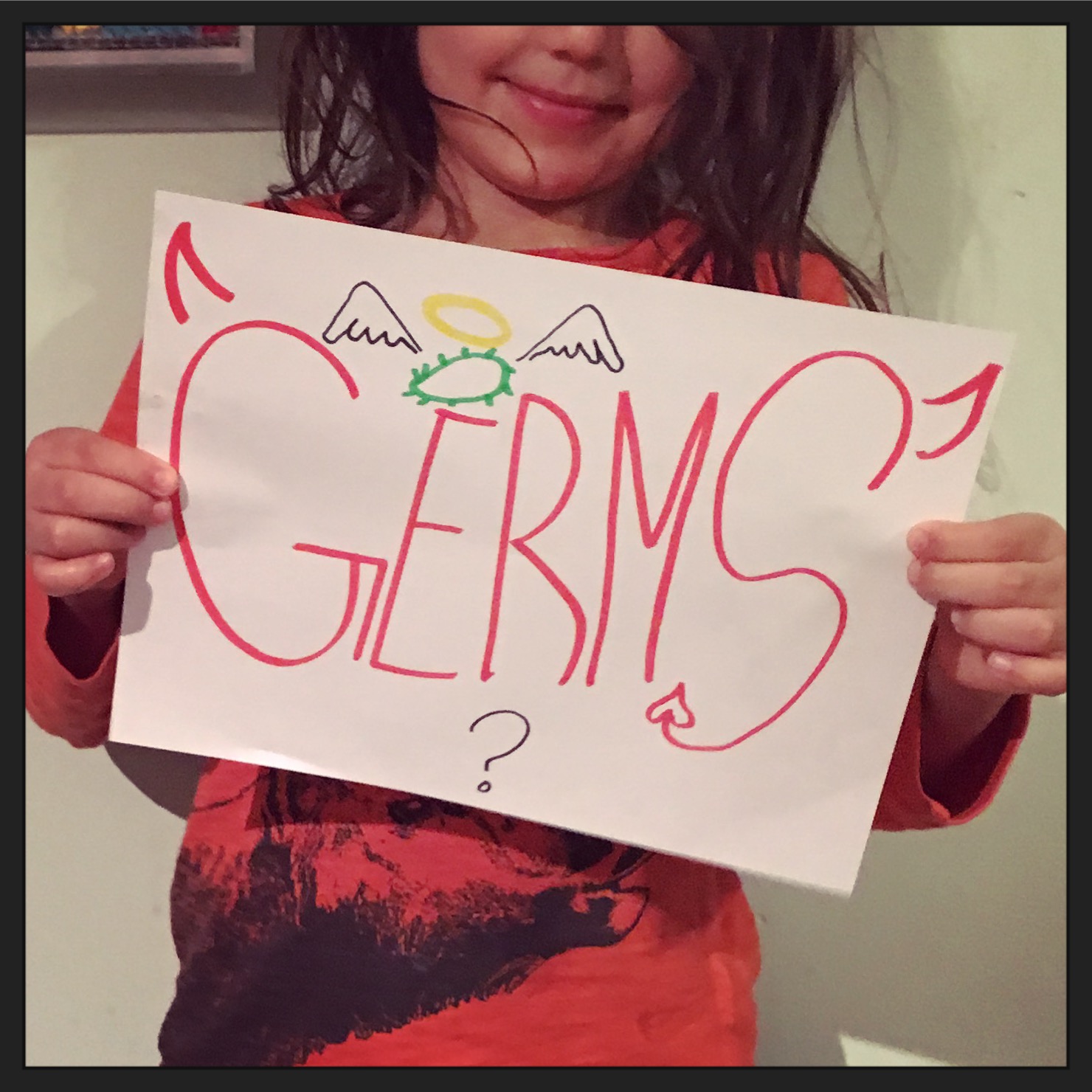
I believe the concept of viewing specific bacteria and other microorganisms which reside in our intestine as beneficial needs to be reviewed and revised. There is no such thing as “good” bacteria—just bacteria that harm you less and outcompete the bacteria that harm you more. So it is not so simple as “good” microbes and “bad” microbes. Yes, it has been shown that certain types of intestinal bacteria can be used to interrupt the implantation—or even kill off—other, more harmful types, such as in the treatment of C. diff. But the reason for the health improvement in this and all other diseases was not the addition of “good” intestinal bacteria, but rather the reduction of the overall microbial population, in conjunction with the relative reduction of specific types, resulting in a more optimal balance. Furthermore, studies have shown that germ-free mice (with no bacteria) are quite healthy, disease free, and live longer lives than their healthy counterparts.8 Of course, living in a germ-free environment is not possible in the real world. The important thing to remember is that, while unhealthy individuals may have too few of some specific types of bacteria to interrupt the overgrowth of others, healthy individuals typically have lower levels of all bacteria.
It’s not simply the presence of “good” bacteria, but rather a healthy balance of intestinal bacteria that’s most important when it comes to your health.
For more information on intestinal bacteria, stay tuned for my next blog post, which will dig deeper to compare the differences between the intestinal microbiome of a generally healthy person versus that of an unhealthy person. For even more info on the latest topics in health and nutrition, sign up for my newsletter.
Want to try a new workout method that’s great for spine health, strength and stability, and flexibility? Join us for ELDOA group classes right here in St. Louis!
References
- Cani PD, Amar J, Iglesias MA, et al. Metabolic endotoxemia initiates obesity and insulin resistance. Diabetes 56, No. 7 (July 2007): 1761-1772. http://diabetes.diabetesjournals.org/content/56/7/1761.full
- Ferrer M, Ruiz A, Lanza F, et al. Microbiota from the distal guts of lean and obese adolescents exhibit partial functional redundancy besides clear differences in community structure. Environ Microbiol 15, No. 1 (Jan 2013): 211-226. http://www.ncbi.nlm.nih.gov/pubmed/22891823
- Bäckhed F, Manchester JK, Semenkovich CF, et al. Mechanisms underlying the resistance to diet-induced obesity in germ-free mice. Proc Natl Acad Sci U S A 104, No. 3 (Jan 2007): 979-984. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1764762/
- Valiquette L, Sirard S, Laupland K. A microbiological explanation for the obesity pandemic? Can J Infect Dis Med Microbiol 25, No. 6 (Nov-Dec 2014): 294-295. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4277155/
- Marri PR, Stern DA, Wright AL, et al. Asthma-associated differences in microbial composition of induced sputum. J Allergy Clin Immunol 131, No. 2 (Feb 2013): 346-352. http://www.ncbi.nlm.nih.gov/pubmed/23265859
- McIntyre CW, Harrison LEA, Eldehni MT, et al. Circulating endotoxemia: a novel factor in systemic inflammation and cardiovascular disease in chronic kidney disease. CJASN 6, No. 1 (Jan 2011): 133-141. http://cjasn.asnjournals.org/content/6/1/133.full
- Sandek A, Bjarnason I, Volk HD, et al. Studies on bacterial endotoxin and intestinal absorption function in patients with chronic heart failure. Int J Cardiol 157, No. 1 (May 2012): 80-85. http://www.ncbi.nlm.nih.gov/pubmed/21190739
- Jones JM, Wilson R, Bealmear PM. Mortality and Gross pathology of secondary disease in germfree mouse radiation chimeras. Radiation Research 45, No. 3 (Mar 1971): 577-588. http://www.jstor.org/stable/3573066?seq=1#page_scan_tab_contents







